Psoriatic Arthritis
 Psoriatic arthritis is an autoimmune joint disease associated with a history of Psoriasis or a family history of Psoriasis. It is classified under Seronegative arthritis’s as there is significant joint symptoms with a background of negative Rheumatoid factor. This condition can be challenging to diagnose and treat as the spectrum of presentation is varied and multiple symptoms can be present. Psoriatic arthritis is seen in around less than 0.1% of the population. Men and women are equally affected with the symptoms starting in 30s and 40s.
Psoriatic arthritis is an autoimmune joint disease associated with a history of Psoriasis or a family history of Psoriasis. It is classified under Seronegative arthritis’s as there is significant joint symptoms with a background of negative Rheumatoid factor. This condition can be challenging to diagnose and treat as the spectrum of presentation is varied and multiple symptoms can be present. Psoriatic arthritis is seen in around less than 0.1% of the population. Men and women are equally affected with the symptoms starting in 30s and 40s.
Around 10-20% of patients who have Psoriasis, develop arthritis with joint pains and swellings. Not all individuals with Psoriasis go on to develop arthritis. Though the term indicates Psoriasis associated arthritis, in some patients arthritis can be the first presentation with the skin lesions developing later in around 15% of the patients. It can present with spine involvement with neck pain or lower back pain as the first symptom with joint pains coming in at a later stage. Plaque psoriasis and psoriasis with nail changes are commonly associated with the development of the arthritis.
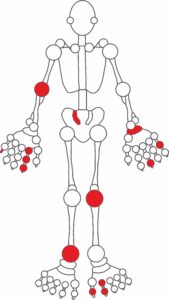
Multiple patterns of symptoms exist. The most common presentation is joint pains with swellings in the hands, knees and feet similar to Rheumatoid arthritis. This condition can also affect the small joints of the fingers and deformities are common. Spinal involvement can be seen similar to the symptoms in Ankylosing Spondylitis. There are a few symptoms which are unique to Psoriatic arthritis such as Sausage like swelling of the fingers called Dactylitis and pain at the tendon insertion sites like sole of the foot or back of the heels. Eye manifestations like painful red eyes are also seen in Psoriatic arthritis.
Joint damage with bony destruction is more, compared to other arthritis and deformities if they occur are irreversible. This condition can be associated with Inflammatory bowel disease also. Smoking is a known risk factor for the increased severity of the joint symptoms and the skin lesions. Treatment response is also reduced in smokers.
Diagnosing Psoriatic arthritis needs careful history and examination especially if there is no obvious associated Psoriasis. Blood tests and X rays can be helpful to know the underlying damage.
Treatment is with medications broadly termed as Disease modifying anti-Rheumatic Drugs “DMARDS”. Medications will be prescribed after careful clinical evaluation. Though side effects can occur, they are rare. These medications were found to be safe in multiple long term clinical studies and will reduce the severity of the joint and the skin symptoms. Biologics are newer group of medications which are being used in cases where adequate clinical response is not achieved. Biologics are relatively safe and have proven efficacy. Early and appropriate treatment is a must as the persistent disease activity can affect the joint’s structure and stability leading to deformities. Even in the absence of active joint symptoms the multisystem organs can be affected leading to long term complications which is prevented by appropriate disease management.